The Slow Progression of Atherosclerosis: Recognizing the Warning Signs
Atherosclerosis, a chronic and progressive condition characterized by the buildup of plaque in the arteries and narrowing of blood vessels, poses a significant threat to cardiovascular health worldwide. Understanding the insidious nature of atherosclerosis is crucial in recognizing its warning signs and taking proactive measures to slow its progression.
This article delves into the intricate details of atherosclerosis, exploring the risk factors that contribute to its development, the early symptoms that may signal its presence, diagnostic tools for accurate detection, lifestyle modifications to mitigate its effects, available medical treatments, and the potential complications of leaving this condition untreated.
By shedding light on the slow progression of atherosclerosis, individuals can empower themselves with knowledge to make informed decisions regarding their heart health and by early detection mitigate its impact on overall well-being.

Table of Contents
ToggleIntroduction to Atherosclerosis
Atherosclerosis is a chronic inflammatory disease characterized by the build-up of fatty deposits, known as plaques, in the walls of arteries. These plaques consist of cholesterol, calcium, and other substances that can obstruct the flow of blood and ultimately lead to serious health complications, such as heart attack and stroke.
The development of atherosclerosis is a complex process that involves multiple factors, including high cholesterol levels, high blood pressure, smoking, and diabetes. Once formed, these plaques can become unstable and rupture, leading to the formation of blood clots that can block blood flow to vital organs.
Understanding the pathophysiology of atherosclerosis is crucial in developing effective prevention and treatment strategies. Current treatment options focus on lifestyle modifications, such as a healthy diet and regular exercise, as well as medications to control cholesterol levels and blood pressure.
In serious situations, surgical procedures like angioplasty or bypass surgery may be needed to improve blood flow to affected areas. As our understanding of the underlying mechanisms of atherosclerosis continues to evolve, new therapeutic targets and interventions are being explored to improve outcomes for individuals at risk of developing this potentially life-threatening condition.
Read more about “The Impact of Myeloid Leukemia on Patients and Families!”
How Atherosclerosis Impacts Cardiovascular Health?
Atherosclerosis is a chronic inflammatory disease characterized by the buildup of plaque in the arterial walls, leading to narrowing and hardening of the arteries. This condition significantly impacts cardiovascular health by increasing the risk of heart attacks, strokes, and other cardiovascular events.
As plaque accumulates, it restricts blood flow to vital organs, causing decreased oxygen and nutrients delivery. This can result in various complications such as angina, arrhythmias, and heart failure.
Additionally, atherosclerosis can lead to the formation of blood clots, which may travel to the brain, causing a stroke, or to the heart, causing a heart attack. Atherosclerosis is a significant cause of heart disease and death globally.
In addition to the physical complications, atherosclerosis also has significant economic implications, as it results in increased healthcare costs for individuals and society.
Preventing and managing atherosclerosis requires lifestyle modifications such as healthy diet, regular exercise, smoking cessation, and stress management.
Moreover, medications such as statins, antiplatelet agents, and blood pressure-lowering drugs are often prescribed to manage risk factors associated with atherosclerosis.
In severe cases, surgical interventions such as angioplasty or bypass surgery may be necessary to restore blood flow to the affected arteries. Therefore, it is crucial for healthcare providers to educate patients on the importance of early detection and intervention to prevent the progression of atherosclerosis and reduce the burden of cardiovascular disease.
Read more about “Understanding the Genetic Factors of Myeloid Leukemia and the Emerging Treatments”
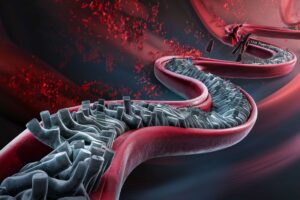
How Plaque Buildup in Arteries Leads to Blockage?
Plaque buildup in arteries, also known as atherosclerosis, is a complex process that can ultimately lead to dangerous blockages. It begins with the accumulation of cholesterol, fats, and other substances in the inner walls of the arteries.
This buildup triggers an inflammatory response, causing the formation of a plaque that narrows the arteries and restricts blood flow. Over time, the plaque can become calcified and hardened, further constricting blood flow and increasing the risk of blockages.
If a blockage occurs, it can prevent oxygen-rich blood from reaching vital organs and tissues, leading to serious health complications such as heart attacks or strokes. Therefore, understanding the mechanisms behind plaque buildup in arteries is crucial in developing effective strategies for prevention and treatment of cardiovascular diseases.
Read more about “What are the Causes and Symptoms of Coronary Artery Disease and How to Treat?”
Risk Factors for Developing Atherosclerosis
There are several key risk factors associated with the development of atherosclerosis. One major risk factor is unhealthy lifestyle choices, such as a diet high in saturated fats, cholesterol, and sodium, as well as physical inactivity.
These habits can lead to the accumulation of cholesterol in the arteries, promoting the formation of plaque. Additionally, smoking is a significant risk factor for atherosclerosis, as it damages the lining of the arteries and accelerates the development of plaque.
Other risk factors include high blood pressure, diabetes, and obesity, all of which can contribute to the progression of atherosclerosis by causing damage to the blood vessels.
Genetic factors also play a role in the development of atherosclerosis, as individuals with a family history of the disease are at a higher risk. Certain genetic mutations can increase the levels of cholesterol in the blood or impair the body’s ability to process and remove cholesterol, leading to the accumulation of plaque in the arteries.
Age and gender are also risk factors, with men being more likely to develop atherosclerosis at a younger age than women. Additionally, certain medical conditions, such as chronic kidney disease and autoimmune disorders, can increase the risk of atherosclerosis by promoting inflammation and damage to the arteries.
Overall, the interplay of lifestyle choices, genetics, and underlying medical conditions all contribute to the development of atherosclerosis and highlight the importance of preventive measures and early intervention in managing the disease.
Read more about “How to Promote Mental Health in LGBTQIA+ Communities?”
Common Symptoms and Warning Signs of Atherosclerosis
The early warning signs of atherosclerosis are often subtle and easily overlooked. One common symptom is chest pain or discomfort, also known as angina. This occurs when the arteries supplying blood to the heart become narrowed, leading to reduced blood flow and oxygen to the heart muscle.
Other symptoms may include shortness of breath, fatigue, and weakness, especially during physical activity. These symptoms may indicate that the arteries are becoming increasingly blocked, and that intervention is necessary to prevent a heart attack or stroke.

As atherosclerosis progresses, it can lead to more severe symptoms and complications. One such complication is peripheral artery disease (PAD), which occurs when the arteries supplying blood to the arms and legs become narrowed. This can cause pain, numbness, and weakness in the affected limbs, as well as skin ulcers and difficulty walking.
Another dangerous complication of atherosclerosis is a stroke, which occurs when plaque buildup in the arteries supplying blood to the brain causes a blockage, cutting off blood flow and oxygen to the brain.
This can result in sudden weakness or numbness on one side of the body, trouble speaking or understanding speech, and vision problems.
It is important to recognize the early warning signs of atherosclerosis and seek medical attention promptly. By catching the condition early, interventions such as lifestyle changes, medication, and medical procedures can be implemented to slow the progression of the disease and reduce the risk of complications.
Individuals at higher risk of atherosclerosis, such as those with a family history of heart disease, high cholesterol, or diabetes, should be especially vigilant in monitoring for symptoms and seeking medical care if necessary.
Early detection and management of atherosclerosis are crucial in protecting heart and vascular health and reducing the risk of serious complications.
How Early Detection and Treatment are Crucial in Preventing Complications?
Early detection and treatment of atherosclerosis is paramount in preventing complications such as heart attack, stroke, or peripheral artery disease. Atherosclerosis is a progressive disease characterized by the buildup of plaque in the arterial walls, narrowing the blood vessels and restricting blood flow to vital organs.
Without timely intervention, this condition can lead to serious cardiovascular events that can be life-threatening. Early detection through screening tests like cholesterol levels, blood pressure measurements, and imaging studies can identify individuals at risk for atherosclerosis before symptoms develop.
Initiating treatment interventions such as lifestyle modifications (diet, exercise), medications (statins, anti-hypertensives), and procedures (angioplasty, stent placement) can help slow down the progression of the disease and reduce the risk of complications.
Therefore, healthcare providers should emphasize the importance of early detection and intervention in managing atherosclerosis to improve patient outcomes and prevent future cardiovascular events.
Diagnostic Tests Used to Identify Atherosclerosis
To diagnose atherosclerosis, various diagnostic tests are used to assess the extent and severity of the disease. One common test is a lipid profile blood test, which measures the levels of cholesterol and triglycerides in the blood.
High levels of cholesterol and triglycerides can contribute to the development of atherosclerosis. Imaging tests such as a coronary calcium scan or carotid ultrasound can also be used to visualize the extent of plaque buildup in the arteries.
In addition to imaging and blood tests, a stress test may be performed to assess how well the heart is functioning under physical stress. This test can help determine if there is reduced blood flow to the heart due to atherosclerosis.
Another important diagnostic test for atherosclerosis is an angiography, where a dye is injected into the arteries to help visualize any blockages or narrowing in the blood vessels.
These diagnostic tests are crucial in identifying atherosclerosis early on and guiding treatment strategies to prevent further complications. Early detection and management of atherosclerosis can help reduce the risk of heart disease and improve overall cardiovascular health.
Complications of Untreated Atherosclerosis
If left untreated, atherosclerosis can result in serious complications such as heart attack, stroke, peripheral artery disease, and even death. The narrowing of arteries restricts blood flow to vital organs, increasing the risk of developing cardiovascular events.
Additionally, atherosclerosis can lead to the formation of blood clots, which can block blood flow to the heart or brain, resulting in a heart attack or stroke. Furthermore, the weakened arterial walls can rupture, causing internal bleeding and potentially fatal consequences.
Therefore, it is crucial to manage and treat atherosclerosis promptly to prevent these severe complications and improve overall health outcomes.
Lifestyle Changes that Can Help Slow the Progression of Atherosclerosis
For individuals diagnosed with atherosclerosis, making positive lifestyle changes is crucial in slowing disease progression and reducing the risk of complications.
Maintaining a heart-healthy diet low in saturated fats, cholesterol, and sodium while incorporating fruits, vegetables, whole grains, and lean proteins can help manage cholesterol levels and prevent plaque buildup in the arteries.
Regular physical activity, such as aerobic exercise and strength training, can also improve cardiovascular health by promoting weight loss, lowering blood pressure, and reducing inflammation in the body.
Smoking cessation is another critical step in preventing further damage to the blood vessels and decreasing the risk of heart attacks or strokes.
Additionally, managing stress through techniques like mindfulness, meditation, or therapy can help reduce tension on the cardiovascular system.
By implementing these lifestyle changes consistently, individuals with atherosclerosis can significantly slow down disease progression and improve their overall health outcomes.
Medications and Procedures Used to Manage Atherosclerosis and Prevent Complications
To manage and prevent this condition, a combination of medications and procedures are often used to prevent complications such as heart attack or stroke.
One commonly prescribed medication is statins, which work by lowering cholesterol levels in the blood and reducing inflammation in the arteries.
Other medications such as antiplatelet drugs (e.g. aspirin) may also be prescribed to prevent blood clots from forming and causing further blockages in the arteries.
In addition to medications, various procedures may be recommended to manage atherosclerosis. One common procedure is angioplasty, in which a balloon is used to widen narrowed arteries and improve blood flow.
In certain situations, a stent might be inserted to assist in maintaining the artery open. Another procedure, known as endarterectomy, involves surgically removing plaque buildup from the inner lining of the artery.
These procedures can help restore blood flow to the affected area and reduce the risk of complications associated with atherosclerosis.
Overall, managing atherosclerosis requires a multidisciplinary approach that may involve a combination of medications and procedures tailored to the individual patient’s needs.
It is important for healthcare providers to work closely with patients to develop a personalized treatment plan that addresses their specific risk factors and symptoms. By effectively managing atherosclerosis, patients can reduce their risk of complications and improve their overall cardiovascular health.
Role of Regular Exercise and Healthy Eating in Preventing Atherosclerosis
Regular exercise and healthy eating play crucial roles in preventing the development and progression of atherosclerosis. Exercise helps to maintain healthy blood pressure, cholesterol levels, and blood sugar control, all of which are important factors in reducing the risk of atherosclerosis.
Additionally, physical activity promotes weight management and overall cardiovascular health, further protecting against the disease. A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help to lower cholesterol levels, reduce inflammation, and provide essential nutrients that support heart health.
By incorporating regular exercise and a balanced diet into daily routines, individuals can greatly reduce their risk of developing atherosclerosis and improve their overall cardiovascular well-being.
Conclusion:
By making necessary lifestyle changes, exploring medical interventions, and understanding the potential consequences of untreated atherosclerosis, individuals can take control of their heart health and improve their quality of life. Remember, knowledge and action are powerful tools in combating this silent threat.
Staying vigilant about the warning signs of atherosclerosis and taking proactive measures to address its underlying causes can significantly reduce the risk of cardiovascular events and improve long-term health outcomes.
By adopting a heart-healthy lifestyle, seeking regular medical evaluations, and following recommended treatment plans, individuals can effectively manage atherosclerosis and optimize their heart health for years to come. Remember, early recognition and intervention are the key against this stealthy disease.
FREQUENTLY ASKED QUESTIONS
1. What are the main risk factors for developing atherosclerosis?
Atherosclerosis, a condition characterized by the build-up of plaque in the arteries, is primarily caused by several main risk factors. First and foremost, a diet high in saturated fats, trans fats, cholesterol, and sugar can significantly increase the likelihood of developing atherosclerosis. Smoking tobacco products also greatly increases the risk due to their damaging effects on blood vessels.
Additionally, individuals with high blood pressure, diabetes, or obesity are more prone to developing atherosclerosis because these conditions put additional strain on the cardiovascular system. Genetic factors can play a role as well; those with a family history of heart disease are more likely to experience plaque accumulation in their arteries.
Lack of physical activity and excessive alcohol consumption also contribute to the risk of developing this serious cardiovascular condition. Management of these risk factors through lifestyle modifications and proper medical treatment is crucial for preventing or slowing down the progression of atherosclerosis.
2. Can atherosclerosis be reversed with lifestyle changes?
Atherosclerosis is a chronic condition commonly associated with lifestyle factors such as smoking, poor diet, lack of physical activity, and obesity. While medical interventions such as medications and surgeries can help manage symptoms and slow disease progression, research suggests that significant changes in lifestyle can potentially reverse atherosclerosis. Adopting a healthy diet rich in fruits, vegetables, whole grains, and lean protein while limiting saturated fats and refined sugars can reduce inflammation and improve cholesterol levels.
Regular exercise has been shown to improve cardiovascular health by strengthening the heart muscle and promoting efficient circulation. Additionally, quitting smoking can prevent further damage to arterial walls.
Combined with medication prescribed by healthcare providers, these lifestyle changes have the potential to halt or even reverse the effects of atherosclerosis over time. It is important for individuals seeking to address this condition through lifestyle modifications to consult with their healthcare provider for personalized recommendations and guidance.
3.What are the typical symptoms of advanced atherosclerosis?
Some typical signs of advanced atherosclerosis include chest pain or angina, shortness of breath, fatigue, weakness, and dizziness. Patients may also experience numbness or weakness in extremities due to decreased blood flow. Additionally, individuals with advanced atherosclerosis may exhibit cognitive decline or memory loss as a result of reduced blood supply to the brain.
Furthermore, individuals may develop peripheral artery disease which can lead to leg pain while walking or even at rest. It is important for patients experiencing these symptoms to seek medical attention promptly as advanced atherosclerosis can increase the risk of serious cardiovascular events such as heart attack or stroke.


