Atherosclerosis V/S Arteriosclerosis and Their Impact on Heart Health!
Atherosclerosis and arteriosclerosis are two closely related but distinct cardiovascular conditions that significantly impact heart and overall cardiovascular health. Understanding the differences between these conditions, their causes, effects, risk factors, implications on the heart is crucial for effective prevention and maintaining optimal cardiovascular health.
This article provides an in-depth knowledge of the pathophysiology, risk factors, clinical manifestations, diagnosis, treatment approaches, and lifestyle modifications related to atherosclerosis and arteriosclerosis, offering valuable insights into maintaining cardiovascular health and reducing the risk of heart disease.
The readers will gain valuable insights into how these conditions affect the heart and what steps can be taken to mitigate their impact on heart health.

Table of Contents
ToggleIntroduction to Atherosclerosis and Arteriosclerosis
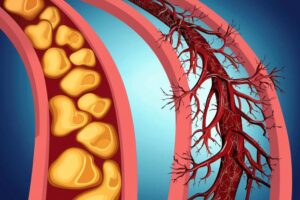
Atherosclerosis and arteriosclerosis are two closely related diseases that affect the cardiovascular system, causing significant morbidity and mortality worldwide. Atherosclerosis refers to the build-up of plaque within the arteries, leading to the narrowing and hardening of the blood vessels.
This process is characterized by the accumulation of cholesterol, fatty deposits, and inflammatory cells on the inner walls of the arteries. As a result, the flow of blood is restricted, which can eventually lead to serious complications such as heart attacks and strokes.
Arteriosclerosis, on the other hand, refers to the general thickening and stiffening of the arterial walls, making them less flexible and more prone to damage. While atherosclerosis is a specific type of arteriosclerosis that involves plaque formation, arteriosclerosis encompasses a broader range of changes that occur in the arteries over time.
Both diseases are closely linked to risk factors such as high blood pressure, high cholesterol levels, smoking, obesity, and a sedentary lifestyle, making them largely preventable through lifestyle modifications and medical interventions.
Understanding the mechanisms underlying atherosclerosis and arteriosclerosis is critical for developing effective prevention and treatment strategies. Research has shown that inflammation plays a key role in the development and progression of these diseases, leading to the formation of vulnerable plaques that are prone to rupture and cause acute cardiovascular events.
By targeting inflammatory pathways and reducing cholesterol levels, healthcare providers can help patients manage their risk of developing atherosclerosis and arteriosclerosis, ultimately improving their cardiovascular health and reducing the burden of cardiovascular disease in the population.
Definition and Causes of Atherosclerosis
Atherosclerosis is a chronic inflammatory disease characterized by the buildup of plaque within the walls of arteries. It is a leading cause of cardiovascular diseases, such as heart attack and stroke. The development of atherosclerosis involves a complex interplay of genetic, environmental, and lifestyle factors.
Over time, the buildup of fatty deposits, cholesterol, calcium, and other substances within the arteries leads to a narrowing and hardening of these blood vessels, impeding the flow of oxygen-rich blood to vital organs.
There are several causes and risk factors that contribute to the development of atherosclerosis. High levels of LDL cholesterol (the “bad” cholesterol) and low levels of HDL cholesterol (the “good” cholesterol) increase the risk of plaque formation in the arteries.
Additionally, factors such as smoking, high blood pressure, diabetes, obesity, and a sedentary lifestyle can accelerate the progression of atherosclerosis. Genetic factors also play a role in the susceptibility to developing this condition. As a result, individuals with a family history of heart disease are at a higher risk of developing atherosclerosis.
In short, atherosclerosis is a complex disease that results from the accumulation of plaque in the arteries, leading to the narrowing and hardening of these blood vessels. Various factors, such as high cholesterol levels, smoking, high blood pressure, diabetes, obesity, and genetic predisposition, contribute to the development and progression of atherosclerosis.
Understanding the causes and risk factors associated with this condition is crucial for implementing preventive measures and interventions to reduce the burden of cardiovascular diseases in the population.
Read more about “Myeloid Leukemia Causes, Symptoms, Prevention and Treatments”
Definition and Causes of Arteriosclerosis
Arteriosclerosis is a chronic condition characterized by the hardening and narrowing of the arteries due to the buildup of plaque on the artery walls. This can lead to decreased blood flow and oxygen delivery to various organs and tissues, increasing the risk of serious health complications such as heart attack, stroke, and peripheral artery disease.
The primary cause of arteriosclerosis is believed to be the accumulation of cholesterol, fat, and other substances in the arterial walls, leading to the formation of plaque. Other factors such as high blood pressure, smoking, diabetes, obesity, and a sedentary lifestyle also contribute to the development of arteriosclerosis.
The process of arteriosclerosis begins with damage to the inner lining of the arteries, which can be caused by high blood pressure, smoking, or high levels of cholesterol in the blood.
This damage triggers an inflammatory response, causing the accumulation of white blood cells and cholesterol in the arterial wall. Over time, these substances form plaque, which hardens and narrows the arteries, restricting blood flow. As the plaque continues to build up, it can eventually block the arteries completely, leading to a heart attack or stroke.
Arteriosclerosis is a progressive condition that can have serious consequences if left untreated. It is important for individuals to adopt a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking, to reduce the risk of developing arteriosclerosis.
Additionally, managing risk factors such as high blood pressure, diabetes, and high cholesterol levels is crucial in preventing the progression of the disease. Early detection and treatment of arteriosclerosis are essential to reduce the risk of complications and improve overall cardiovascular health.
Read more about “What are the Causes and Symptoms of Peripheral Artery Disease and how to treat?”
Key Differences Between Atherosclerosis and Arteriosclerosis
Atherosclerosis and arteriosclerosis are both chronic conditions that affect the cardiovascular system, but they differ in their specific mechanisms and consequences. Atherosclerosis is characterized by the blockage of the arteries due to fat, cholesterol, calcium, and other substances accumulation. This narrowing of the arteries can restrict blood flow and increase the risk of heart attack and stroke.
On the other hand, arteriosclerosis refers to the hardening and thickening of the arterial walls, which can make the arteries less flexible and more prone to damage. This stiffening of the arteries can increase blood pressure and also raise the risk of cardiovascular events.
Another key difference between atherosclerosis and arteriosclerosis lies in their causes and risk factors. Atherosclerosis is often associated with factors such as high cholesterol, high blood pressure, smoking, and a sedentary lifestyle.
The buildup of plaque in the arteries is a gradual process that can be influenced by diet and lifestyle choices. In contrast, arteriosclerosis is more closely linked to aging and genetic factors. As individuals grow older, their arteries naturally become less elastic and more prone to hardening.
While lifestyle modifications can help prevent or slow down the progression of atherosclerosis, arteriosclerosis may be more difficult to reverse once it has developed. Understanding these key differences is essential for developing effective prevention and treatment strategies for these complex cardiovascular conditions.
Read more about “What are the Causes and Symptoms of Periodontitis and how to Treat?”
Understanding the Pathophysiology of Atherosclerosis
Atherosclerosis is a complex disease process that involves the accumulation of plaque within the arterial walls, leading to narrowing and hardening of the arteries. It is a multifactorial disease with several contributing factors, including chronic inflammation, lipid deposition, and endothelial dysfunction.
The initial step in the pathophysiology of atherosclerosis is the endothelial injury, which triggers an inflammatory response and promotes the adhesion of circulating monocytes to the damaged endothelium.
These monocytes then differentiate into macrophages, which engulf low-density lipoprotein (LDL) particles and form foam cells, contributing to the formation of fatty streaks. Over time, these fatty streaks can progress into more advanced lesions, resulting in the development of atherosclerotic plaques.
As the atherosclerotic plaques continue to grow, they can lead to the narrowing of the arteries and obstruct blood flow, increasing the risk of cardiovascular events such as heart attacks and strokes.
The pathophysiology of atherosclerosis also involves the activation of various pro-inflammatory pathways, including the release of cytokines and growth factors that promote the proliferation of smooth muscle cells and fibrous tissue within the plaques. Additionally, the rupture of these unstable plaques can trigger the formation of blood clots, further compromising blood flow to vital organs.
Understanding the pathophysiology of atherosclerosis is crucial for developing effective prevention and treatment strategies, as targeting the underlying mechanisms of the disease can help reduce the burden of cardiovascular disease in individuals at risk.
Read more about “How to Cope with Depression in LGBTQIA+ Communities?”
Understanding the Pathophysiology of Arteriosclerosis
Arteriosclerosis, a condition characterized by the hardening and narrowing of arteries, is a key contributor to cardiovascular disease, the leading cause of death globally.

The pathophysiology of arteriosclerosis involves a complex interplay of various mechanisms, including inflammation, lipid accumulation, and smooth muscle cell proliferation. Initial damage to the arterial wall triggers an inflammatory response, leading to the recruitment of immune cells such as macrophages and T cells.
These immune cells release pro-inflammatory cytokines and growth factors, promoting the migration of smooth muscle cells from the media to the intima layer of the artery.
This migration, coupled with the accumulation of cholesterol and other lipids, forms fatty streaks that eventually progress into atherosclerotic plaques. As the plaques grow, they can disrupt blood flow and lead to complications such as thrombosis and myocardial infarction.
Understanding the pathophysiology of arteriosclerosis is crucial for the development of effective interventions, such as lifestyle modifications, medications, and surgical procedures, aimed at preventing or reducing the progression of the disease.
Future research efforts should focus on further elucidating the molecular mechanisms underlying arteriosclerosis to identify novel therapeutic targets and improve patient outcomes.
Elastic Fiber Degradation and Stiffening of Arteries
The degradation of elastic fibers in the arterial walls is a hallmark of aging and various cardiovascular diseases, leading to progressive stiffening of the arteries. Elastic fibers, predominantly composed of elastin and fibrillin, play a crucial role in providing elasticity and resilience to the arterial walls, allowing for cohesive expansion and contraction during each cardiac cycle.
However, with advancing age and the presence of risk factors such as hypertension and diabetes, there is an increased production of matrix-degrading enzymes such as matrix metalloproteinases (MMPs), which target and degrade elastin fibers.
This enzymatic degradation results in the loss of elasticity and compliance of the arterial walls, leading to stiffening and increased vascular resistance, ultimately contributing to the development of hypertension, arterial stiffness, and cardiovascular events.
The stiffening of arteries due to elastic fiber degradation has profound implications on cardiovascular health and disease progression. Increased arterial stiffness not only impairs the ability of arteries to buffer blood pressure fluctuations but also alters the transmission of pulsatile flow from the heart to the peripheral tissues, leading to increased cardiac workload and reduced perfusion to vital organs.
Furthermore, stiffened arteries are associated with elevated systolic blood pressure, reduced diastolic perfusion, and impaired endothelial function, all of which are key contributors to the development of atherosclerosis, stroke, and heart failure.
Therefore, understanding the mechanisms underlying elastic fiber degradation and arterial stiffening is crucial for the development of targeted therapies aimed at preserving arterial elasticity and function, ultimately mitigating the progression of cardiovascular diseases.
Impact of Atherosclerosis on Heart Health
Atherosclerosis is a chronic inflammatory disease characterized by the accumulation of plaque in the arterial walls, leading to narrowing and hardening of the blood vessels. This condition significantly impacts heart health by reducing blood flow to the heart muscle, thereby increasing the risk of coronary artery disease and heart attacks.
As the plaque builds up in the arteries, it restricts the flow of oxygen-rich blood to the heart, causing chest pain (angina) and potentially leading to a heart attack if the blood flow is completely blocked. Moreover, atherosclerosis can also lead to the formation of blood clots, which can further obstruct the blood vessels and trigger a heart attack or stroke.
The impact of atherosclerosis on heart health is profound and can have serious consequences if left untreated. Lifestyle factors such as smoking, high cholesterol, high blood pressure, diabetes, and a sedentary lifestyle can increase the risk of developing atherosclerosis and exacerbate its effects on heart health.
It is crucial for individuals to adopt healthy habits such as regular exercise, a balanced diet, quitting smoking, and managing chronic conditions to prevent the progression of atherosclerosis and reduce the risk of cardiovascular events.
Additionally, early detection and proper management of atherosclerosis through medications, lifestyle modifications, and surgical interventions can help improve heart health and reduce the risk of complications associated with this condition.
Impact of Arteriosclerosis on Heart Health
Arteriosclerosis is a condition characterized by the hardening and narrowing of the arteries, which can have a significant impact on heart health. As these arteries become more rigid and clogged with plaque, it becomes increasingly difficult for blood to flow freely to the heart.

This can lead to a variety of cardiovascular issues, including high blood pressure, coronary artery disease, and even heart attacks. The reduced blood flow can also limit the amount of oxygen and nutrients that the heart receives, leading to a weakened and strained heart muscle.
In addition to the physical effects on the heart, arteriosclerosis can also have a profound impact on overall heart function and efficiency. Because the arteries are narrowed and hardened, the heart has to work harder to pump blood throughout the body.
This increased strain can lead to a variety of symptoms, including fatigue, shortness of breath, and even chest pain. Over time, this continuous overexertion can weaken the heart muscle and increase the risk of heart failure.
Therefore, it is crucial for individuals with arteriosclerosis to manage and monitor their condition closely, through lifestyle modifications, medication, and regular medical check-ups, in order to prevent further damage to their heart health.
Risk Factors for Atherosclerosis and Arteriosclerosis
Atherosclerosis and arteriosclerosis are two related conditions that involve the narrowing and hardening of arteries, leading to an increased risk of cardiovascular disease. Atherosclerosis is a specific type of arteriosclerosis characterized by the buildup of plaques in the arterial walls.
Risk factors for these conditions include both modifiable and non-modifiable factors. Non-modifiable risk factors for atherosclerosis and arteriosclerosis include age, family history, and genetics.
Individuals over the age of 45-years with a family history of cardiovascular disease are at a higher risk of developing these conditions. Modifiable risk factors for atherosclerosis and arteriosclerosis include smoking, a high cholesterol diet, obesity, lack of physical activity, and poorly managed diabetes.
Smoking is one of the most significant risk factors for these conditions, as it damages the lining of the arteries and accelerates the buildup of plaques.
Preventative measures for atherosclerosis and arteriosclerosis include maintaining a healthy diet low in saturated fats, engaging in regular physical activity, avoiding smoking and excessive alcohol consumption, and managing conditions such as high cholesterol and diabetes.
Regular exercise helps to maintain a healthy weight and reduce cholesterol levels, while a diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent the buildup of plaques in the arteries.
Managing conditions such as high blood pressure and diabetes through medication and lifestyle changes can also help reduce the risk of atherosclerosis and arteriosclerosis. Overall, understanding and addressing risk factors for these conditions is essential for maintaining cardiovascular health and reducing the risk of heart disease and stroke.
Diagnosis and Screening for Atherosclerosis & Arteriosclerosis
Atherosclerosis and arteriosclerosis are both diseases that affect the arteries, leading to serious cardiovascular complications. Diagnosis and screening for these conditions typically involve a combination of medical history assessment, physical examination, and laboratory tests.
One common diagnostic tool is the use of imaging techniques such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) to visualize plaque buildup in the arteries. Additionally, blood tests can measure levels of cholesterol and other lipid markers associated with increased risk of developing atherosclerosis.
Screening guidelines recommend routine monitoring of blood pressure, cholesterol levels, and overall cardiovascular health starting at a young age to identify early warning signs of atherosclerosis and arteriosclerosis before they progress to more severe complications such as heart attack or stroke.
Early detection through comprehensive screening can enable healthcare professionals to implement preventative measures such as lifestyle modifications or medication management to reduce the risk of cardiovascular events in at-risk individuals.
Clinical Manifestations and Complications of Atherosclerosis & Arteriosclerosis
Clinical manifestations of atherosclerosis and arteriosclerosis can include chest pain (angina), shortness of breath, fatigue, and heart palpitations which can progress to more serious conditions such as myocardial infarction (heart attack) or stroke.
As the plaques continue to grow and narrow the arteries, complications may arise including hypertension, peripheral artery disease, aneurysms, and even organ damage if blood flow is severely restricted.
Additionally, individuals with atherosclerosis and arteriosclerosis are at an increased risk for developing blood clots which can further exacerbate their condition.
It is crucial for healthcare professionals to identify these clinical manifestations early on, in order to prevent potentially life-threatening complications and improve patient outcomes through lifestyle modifications, medication therapy, or surgical interventions.
Prevention and Treatment Options for Atherosclerosis & Arteriosclerosis
Prevention plays a crucial role in managing these conditions, including lifestyle modifications such as regular exercise, maintaining a healthy diet low in saturated fats and cholesterol, quitting smoking, and managing stress levels.
Furthermore, medications such as statins, which help lower cholesterol levels, can be prescribed to reduce the buildup of plaque in the arteries.
In severe cases where blockages are causing significant symptoms or complications, surgical interventions such as angioplasty or bypass surgery may be necessary to restore adequate blood flow.
Overall, early detection and intervention are key in effectively managing atherosclerosis and arteriosclerosis to prevent further complications and improve overall cardiovascular health.
Lifestyle Changes to Manage Atherosclerosis and Arteriosclerosis
Managing atherosclerosis and arteriosclerosis through lifestyle changes is crucial in preventing progression of cardiovascular disease. Implementing a healthy diet low in saturated fats, cholesterol, and processed foods while incorporating fruits, vegetables, whole grains, and lean proteins can help reduce plaque buildup in the arteries.
Regular exercise is also essential for maintaining cardiovascular health, as physical activity can improve blood flow, lower cholesterol levels, and decrease inflammation. Additionally, quitting smoking and limiting alcohol consumption are important lifestyle modifications to reduce the risk of developing or worsening arterial diseases.
By adopting these lifestyle changes and working closely with healthcare professionals to monitor progress, individuals with atherosclerosis and arteriosclerosis can effectively manage their condition and improve overall heart health.
Conclusion:
Atherosclerosis and arteriosclerosis pose significant challenges to heart health, but with early detection, proper management, and lifestyle modifications, individuals can take proactive steps to safeguard their cardiovascular well-being. By staying informed about these conditions and adopting healthy habits, individuals can reduce their risk of heart disease and enjoy a higher quality of life.
Remember, a proactive approach to heart health is key to preventing the progression of atherosclerosis and arteriosclerosis, ultimately leading to a healthier heart and a happier life.
FREQUENTLY ASKED QUESTIONS
1. What is the main difference between atherosclerosis and arteriosclerosis?
The main difference between these two conditions lies in their underlying causes and pathophysiology. Atherosclerosis specifically refers to the buildup of plaque within the arterial walls, consisting of cholesterol, fatty deposits, inflammatory cells, and calcium. This buildup can eventually lead to narrowing or blockage of the arteries, restricting blood flow to vital organs. On the other hand, arteriosclerosis is a more generalized term that encompasses any thickening and hardening of the arterial walls due to factors such as aging, high blood pressure, or diabetes.
While atherosclerosis is a subset of arteriosclerosis, it is characterized by a distinct process involving plaque formation and inflammation within the arteries. Both conditions can have serious consequences for cardiovascular health if left untreated, making early detection and management crucial in preventing complications like heart attacks or strokes.
2. Are there any specific symptoms to watch out for in atherosclerosis and arteriosclerosis?
While they share similar characteristics, there are some specific symptoms to watch out for in each condition. In atherosclerosis, symptoms may include chest pain or angina, shortness of breath, weakness or dizziness, and even stroke or heart attack if left untreated. On the other hand, arteriosclerosis often presents with symptoms such as leg pain while walking (claudication), cold extremities, high blood pressure, and an increased risk of developing peripheral artery disease.
It is important to note that these symptoms can vary widely from person to person, so it is crucial to seek medical attention if you experience any concerning signs or risk factors for cardiovascular disease. Regular check-ups and screenings can help detect these conditions early on and prevent further complications.
3. How can lifestyle changes like diet and exercise help in managing atherosclerosis and arteriosclerosis?
Lifestyle modifications, such as adopting a healthy diet and regular exercise regimen, play a crucial role in managing atherosclerosis and arteriosclerosis. A diet high in fruits, vegetables, whole grains, and lean proteins can help lower cholesterol levels and reduce the build-up of plaque in the arteries. Additionally, incorporating foods rich in omega-3 fatty acids, such as fish and nuts, can help decrease inflammation and improve overall heart health.
Engaging in regular physical activity promotes weight loss, lowers blood pressure, and improves circulation—all of which are key factors in preventing the progression of these cardiovascular diseases. By making sustainable lifestyle changes that emphasize nutritious eating habits and consistent exercise routines, individuals can effectively manage atherosclerosis and arteriosclerosis while promoting long-term cardiovascular health. It is recommended to consult with a healthcare provider or registered dietitian for personalized recommendations tailored to individual needs.


